
They may report sitting on the toilet for hours at a time to let urine dribble from their bladders more or less continuously, to keep the bladder as empty as possible and thus minimize pain. Patients may describe the pain as ranging from a mild burning sensation to severe and debilitating. Many clinicians use the Pelvic Pain, Urgency, and Frequency (PUF) questionnaire as a screening and diagnostic tool. When one of these comorbid conditions flares or causes symptoms, the patient also may have a flare or exacerbation of IC. IC patients commonly have several diagnoses, such as irritable bowel syndrome, endometriosis, vulvodynia, migraine, fibromyalgia, dyspareunia, increased pain during the luteal phase of the menstrual cycle, or dysmenorrhea. Urinary frequency occurs because voiding partially or completely relieves the pain caused by bladder filling thus, patients prefer to maintain low bladder volumes. The pain, which originates from the bladder, usually is felt suprapubically.
Painful bladder syndrome dietary modification pdf#
(See Conditions that may mimic IC by clicking on the PDF icon above.) IC always causes pain associated with bladder filling or emptying, usually accompanied by urinary frequency, urgency, and nocturia. IC diagnosis rests on characteristic signs and symptoms and exclusion of other possible causes. This protein may prevent growth of healthy new bladder cells and prevent bladder cells from repairing the damaged bladder lining. Bladder mast cells also may play a role in proliferation of ongoing bladder damage after the initial injury.Ī third theory involves antiproliferative factor (APF)-a unique protein found in urine in the bladder of IC patients. This process may promote further tissue damage, pain, and hypersensitivity.
According to this theory, defects in the GAG layer may allow urinary irritants to penetrate and activate underlying nerve and muscle tissues.

Experts don’t know whether these abnormalities are primary or arise secondary to another (unrecognized) condition.Ī second theory involves the glycosaminoglycan (GAG) layer, which normally coats the surface lining of the bladder, making it impermeable to solutes. Many studies show that IC patients have bladder-lining abnormalities, which may appear in biopsies.
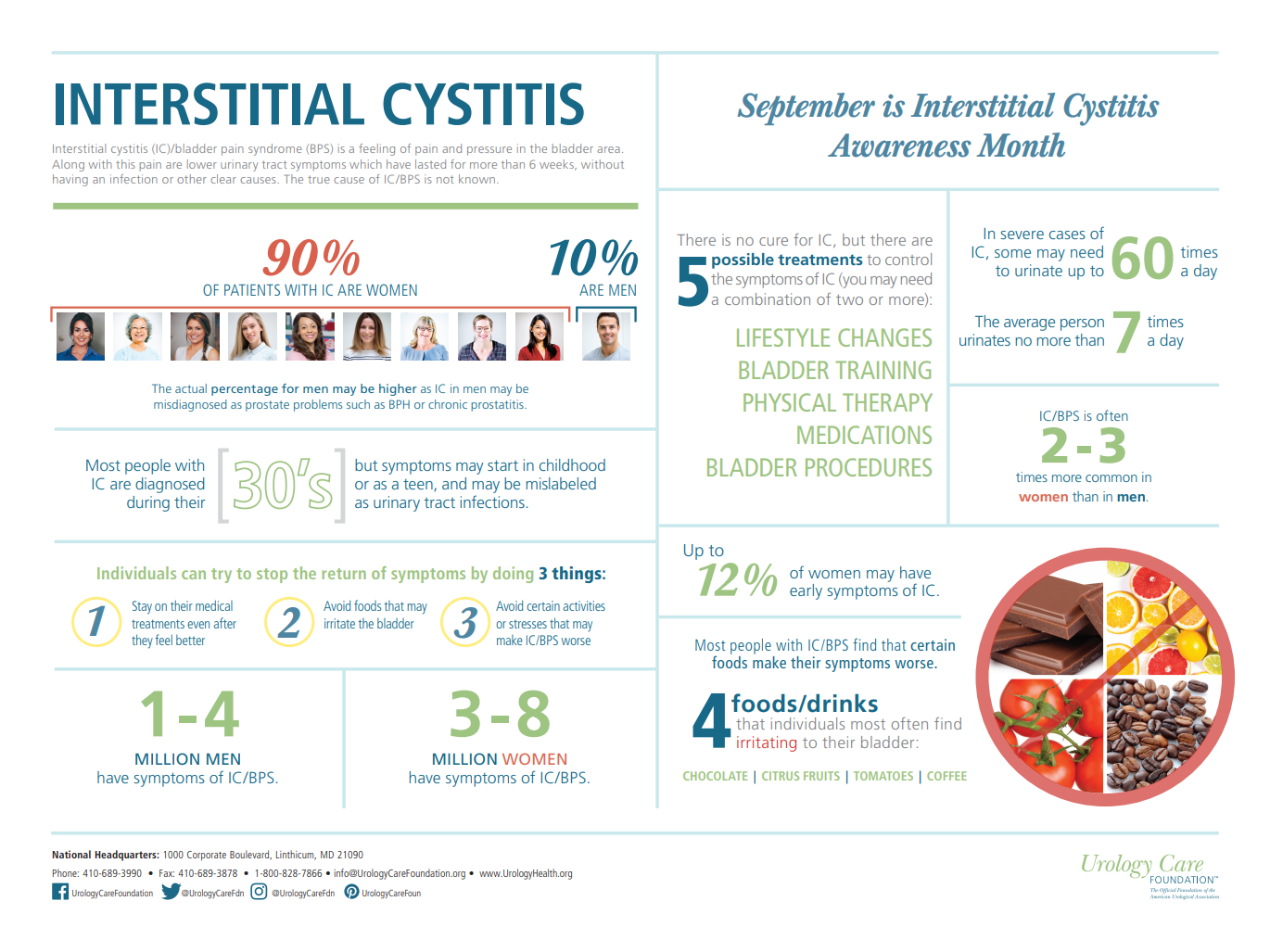
According to one theory, injury to the bladder’s inner protective mucous lining causes leakage of urinary chemicals (such as potassium) into surrounding tissues, resulting in pain and bladder irritation. Several pathogenic mechanisms have been proposed to explain IC. IC can start in childhood, although studies haven’t been done to establish its prevalence in this age group. However, that number is probably lower than the true rate because IC in men may be mistaken for another disorder, such as chronic prostatitis or chronic pelvic pain syndrome. Findings from the Boston Area Community Health (BACH) survey show that roughly 1 to 4 million men have IC. According to the RAND IC Epidemiology (RICE) Study, the largest IC epidemiology study undertaken, about 3 to 8 million women in the United States (roughly 3% to 6% of all women) may have IC. New research indicates IC is more prevalent than originally thought. Diagnosis and treatment can be controversial, and for many patients, the treatment is complicated. Pain commonly occurs in the general pelvic region, inguinal area, inside of the thighs, in the labia or vaginal lips, deep inside the vagina, urethra, clitoris, and in the perineum. They void frequently to decrease pain by eliminating urine in the bladder. Many patients with IC have pain on bladder filling and urination, as well as with sexual intercourse. Also called painful bladder syndrome, IC is marked by pelvic and bladder pain of varying severity and lasting for an extended time, along with urinary frequency. Cranford’s symptoms? Most likely, you’d place interstitial cystitis (IC) at the top of your list.
Which condition would you suspect as the cause of Ms. The pain increases when her bladder is full, isn’t relieved when she voids, and isn’t cyclic or timed with her menstrual cycle. She reports pain during and after sexual intercourse, which at times has deterred her from having sex. She says she has been voiding 20 or more times per day for the past year. Carole Cranford, age 52, comes to the outpatient clinic complaining of pain and pressure in the bladder area, which she rates as a 10 on a 1-to-10 scale, as well as urinary urgency and frequency.


 0 kommentar(er)
0 kommentar(er)
